Viral Aerosol
Panic was spreading through continents faster than the COVID-19 pandemic was spreading, conquering more and more countries. And let anyone who was not afraid of getting this new disease throw a stone at me, especially given the unprecedented anti-epidemic measures that were being taken in China. It was important to understand this unknown process as soon as possible.
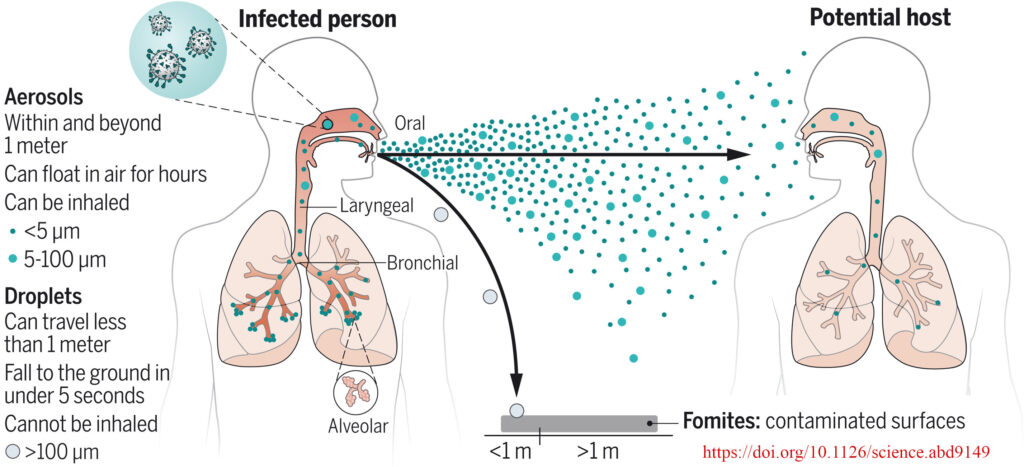
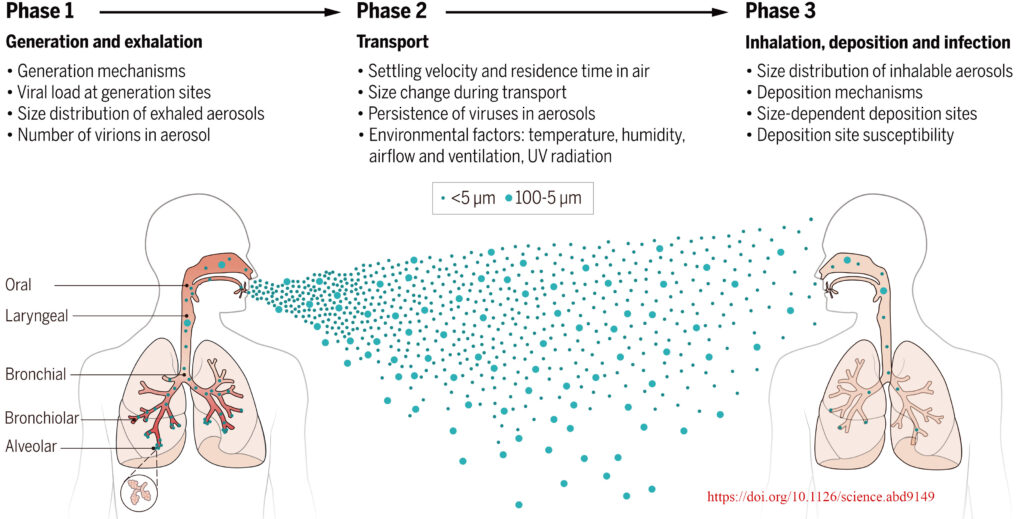
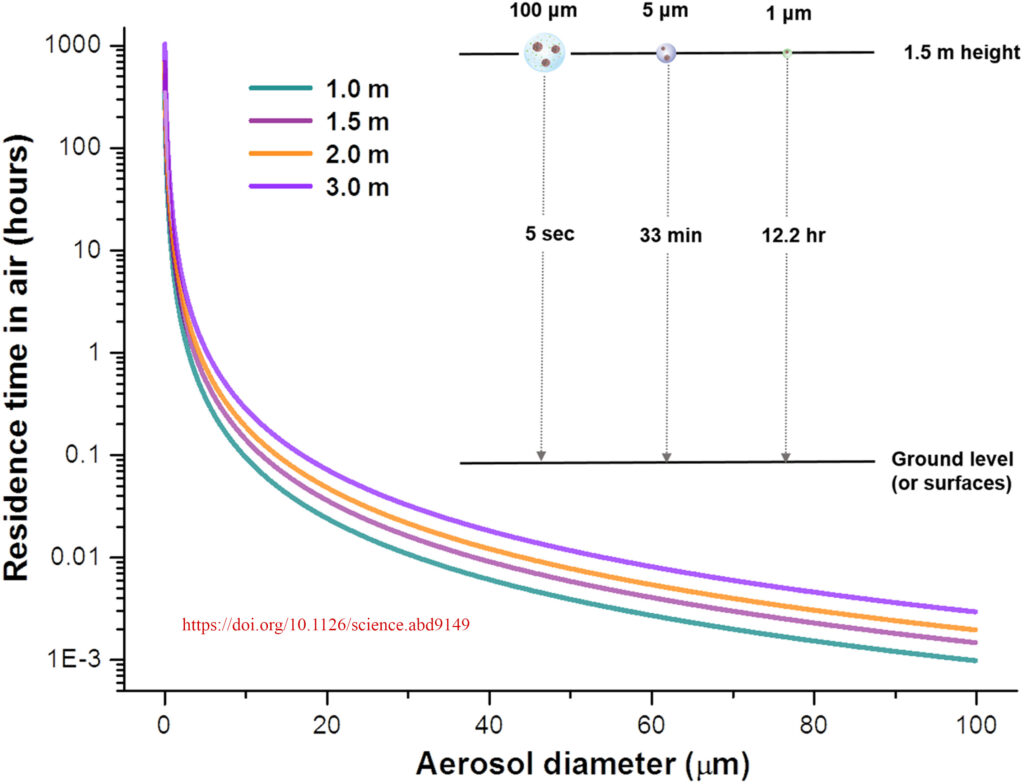
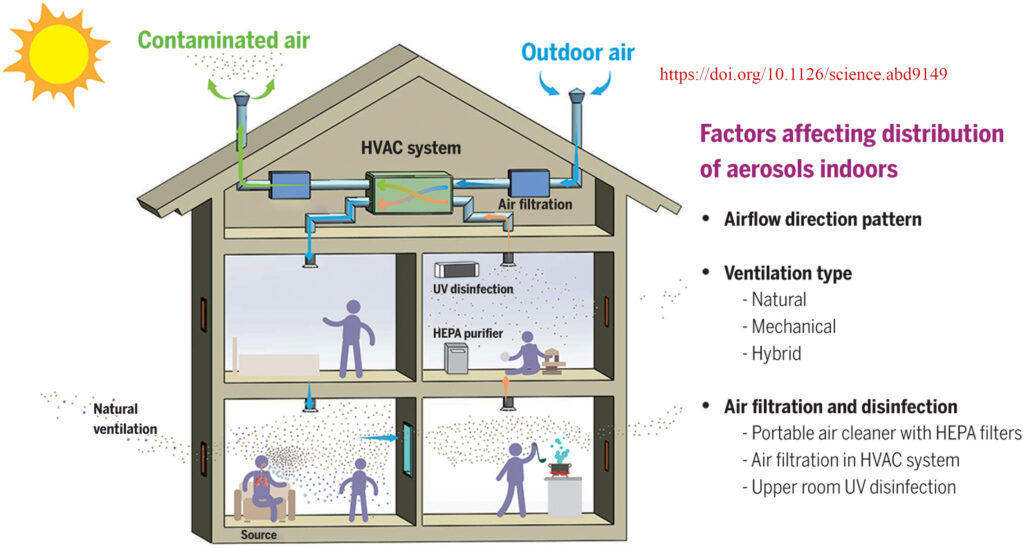
The search carried out in the world’s scientific information databases made it possible to get acquainted with serious publications in peer-reviewed internationally recognized journals on the epidemiology, clinic, pathophysiology of COVID-19, virology, origin and mutation of the SARS-CoV-2 virus, and the resistance of this virus to survival in the body of an infected person and in the environment. My attention was drawn to a review article written by a group of experts from Taiwan (People’s Republic of China), Israel, and the United States (Wang Ch.C., Prather K.A., Sznitman J., Jimenez H.L., Lakdawala S.S., et al. Airborne transmission of respiratory viruses // Science. 2021 Aug 27. Vol. 373. 6558. eabd9149. DOI: https://doi.org/10.1126/science.abd9149). The article is based on a thorough analysis of more than 200 original publications in peer-reviewed journals that investigate the problems of the formation of fine infected aerosol in the respiratory organs of a person with COVID-19, possible ways of its spread in the environment and indoors, the effectiveness of various types of protective masks, the degree of penetration of aerosol particles into the human respiratory system, including those infected with the SARS-CoV2 virus. For decades, it has been believed that severe acute respiratory syndrome (SARS) are transmitted by airborne droplets. It was believed that droplets formed during sneezing or coughing of a sick person get on the mucous membranes of a healthy person (eyes, lips, mouth, and nasopharynx). Epidemiological investigations of COVID-19 outbreaks have suggested that there is a mechanism for the transfer of the infectious agent over quite long distances within not only one room but the entire building. Experimentally, it has been confirmed that a person releases fine particles less than 100 microns in size not only when sneezing or coughing, but also when breathing, talking, singing, or screaming. While droplets larger than 100 microns stay in the air for no more than 5 seconds and fall to the floor and surrounding surfaces under the influence of gravity, aerosol particles smaller than 5 microns can remain in relatively still room air for hours. In the presence of air currents, such particles are transported over long distances not only within the room itself but also through leaks or the ventilation system within the building, even to other floors. Most researchers present evidence that SARS-CoV-2 and other viruses can spread over distances greater than the recommended 2 m in poorly ventilated rooms.
Under the pressure of experimental and epidemiological studies, the World Health Organization (WHO) and the US Centers for Disease Prevention (CDC) have recognized the aerosol route of human-to-human transmission of SARS-CoV-2 as the main route of transmission.
Approximately 20% to 45% of people infected with SARS-CoV-2 do not show symptoms. Some researchers suggest that such people have low levels of virus concentration in the aerosols and saliva droplets they generate and therefore pose a lower risk of infection to others than people with severe symptoms.
One of the most effective ways to protect against the transmission of viruses from a patient is to use protective masks. Both field studies and special modeling experiments on dummies have shown that all masks can reduce to some extent the flow of not only large droplets of saliva but also fine particles smaller than 5 microns into the surrounding space. The most effective in this regard are protective masks No. 95, followed by surgical masks, and then various fabric masks. However, it should be noted that masks do not provide 100% protection. Therefore, in hospitals with COVID-19 patients, staff should be provided with personal protective equipment. Poor fit of any mask to the human body (face, neck, forehead) significantly impairs its effectiveness. The same can be said about protecting the respiratory system of a healthy person from viral aerosol contamination generated by patients with acute respiratory viral infections.
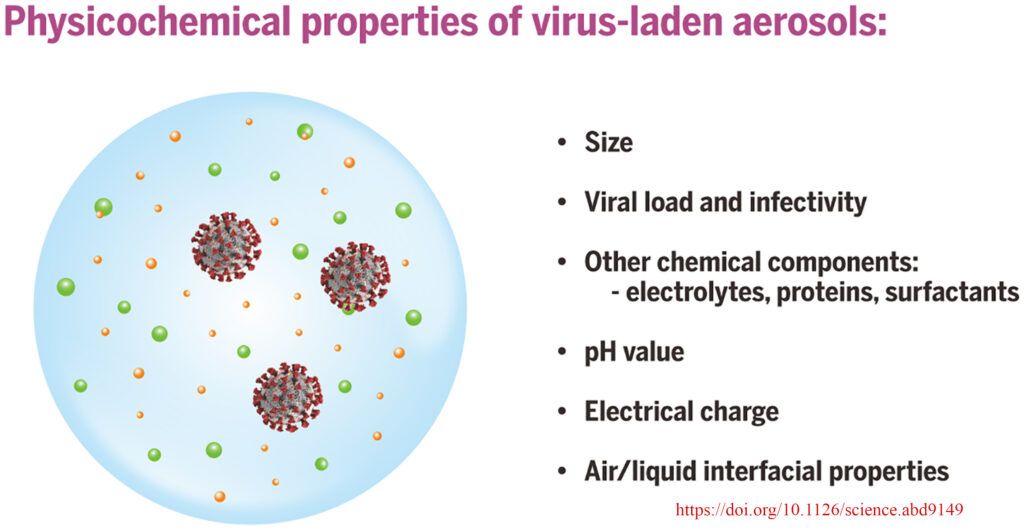
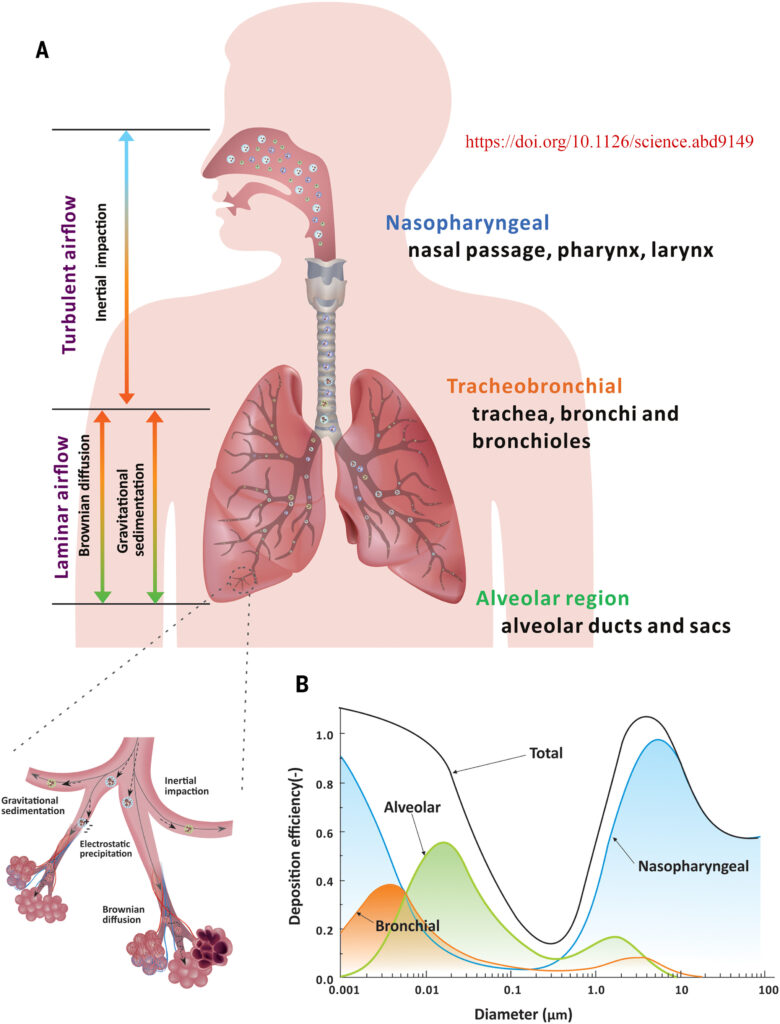
The length of time a virus survives in an aerosol particle depends on its composition and the impact of environmental factors such as air temperature and humidity, and the intensity of ultraviolet radiation. Various viruses, or their traces, are detected more often in aerosol particles of less than 5 microns. While particles larger than 10 microns are retained in the upper respiratory tract, particles smaller than 5 microns reach the alveoli and bronchioles. A nasally administered dose of viruses is less effective in causing infection than a dose that penetrates deeper into the airways, up to the alveoli.
Visualizing the plume of aerosol particles formed by a person’s breathing is enough to recall a frosty day when water vapor contained in the exhaled air condenses and forms a kind of foggy plume. The only difference is that the aerosol of a sick person, although invisible, does not disappear in the room. In case of poor ventilation, it also accumulates because it hangs in the air for a long time. More people mean more aerosol, and you are more likely to inhale infected aerosol, especially when you enter a room where a person with SARS has just been. Viruses can survive in this aerosol for 1 to 3 hours. In large cities with multi-story buildings, elevators can be such rooms. Supermarkets, cinemas and theaters, and indoor stadiums are out of the question in this regard. They can serve as a place for the spread of any viral infection.
The so-called small architectural forms (SAFs), which house shops, hairdressers, etc., also have a negative effect. As a rule, they have poor ventilation, which further contributes to the spread of viral infections.
At one time, aero-ionizers were very popular thanks to the work of O.L. Chizhevsky, O.O. Minh, Y.D. Dumansky, M.G. Shandala, and many other scientists experimentally proved the extremely important role of negatively charged oxygen ions in the vital activity of living organisms. Since ionization is carried out through an electric discharge, the bactericidal effect of the device is enhanced. The aero-ionizer restores the concentration of negatively charged oxygen ions to their original (natural) value, which corresponds to their concentration in open space (in the field, in the forest, etc.). It should be remembered that during the SARS epidemic, it is not recommended to use them in the presence of people, especially those with SARS, as a charged aerosol is better retained in the human respiratory tract. And if this aerosol contains an infectious agent, the consequences are quite obvious.
To understand how air flows behave in an apartment in a high-rise building, you need to know the following. Ventilation is based on the so-called natural inducement due to the difference in temperature between the outside and inside air. Exhaust openings in the apartment are located in the kitchen, toilet, and bathroom. Most of the time, there is no organized air flow in the apartment. If the doors and windows are tightly closed, the ventilation does not work. When a window or door is open, colder air from the outside enters the room, sinks towards the floor, and goes to the ventilation grilles in the kitchen, bathroom, and toilet. This process is much more complicated, but this is not the place or time to dwell on it. The above suggests that when ventilating a room with a SARS patient, it is advisable not to stay for a long time in these air streams, where there is a high probability of fine infected aerosol (we realize the conventionality of such terms as infected and viral aerosol).
Emphasizing the predominantly aerosolized mechanism of transmission of respiratory viral infections both near a sick person and at a distance, the authors of the article do not dismiss the importance of the spread of these diseases through droplets and fomites. The fight against the spread of SARS should take into account all these mechanisms.
Sunlight is still recommended as an effective means of combating microbial and viral contamination of indoor air. But we have to disappoint the supporters of indoor insolation. The sun’s ultraviolet radiation, which has passed through two layers of silicate glass, not to mention glass with different metal oxide coatings, does not transmit ultraviolet radiation of such a spectrum and power that can act bactericidally. This statement of mine is based on my research and contradicts the information contained in this article, which I am now presenting to you. The sun’s ultraviolet radiation outside the house is capable of destroying viruses and germs, but in the geographical latitudes of Ukraine only during the warm months of the year. Therefore, some researchers reasonably believe that the seasonality of SARS is related to this.
On our website, I have already published a popular science article about other mechanisms of aerosol formation in the air of an apartment and its potential threat to human health (https://health.gov.ua/activity/scientific-educational-activity/dust-in-homes-influence-on-health/ A MULTIFACETED ENEMY OF HEALTH IN THE HOME).
The results of a study of the mechanisms of aerosol formation in different parts of the respiratory tract from the alveoli to the oral cavity led scientists to believe that breathing, talking, singing, crying, and screaming of an infected person is likely to release more viral aerosol by a sick person in general than a less frequent cough.
Staying for more than an hour in poorly ventilated, crowded rooms (theaters, churches, cruise ships, etc.) in the presence of a patient with SARS among this contingent significantly increases the risk of infection.
Perhaps no one needs to be convinced that not only COVID-19, influenza, and other SARS cause severe damage to public health every year, both in terms of overloading the health care system and the economic costs of treating patients, sick leave, lost production, etc. There is no doubt that in light of the data on the spread of viral infections through the aerosol route in the premises, approaches to the design of ventilation in residential, especially public buildings, should be changed.
The aerosol, let’s call it conventionally, the plume from each person should be picked up in public areas by the airflow going from the bottom up from the lower air inlets to the outlets near the ceiling. This will make it impossible for the infectious aerosol to spread horizontally across the room where other people are.
When the fight against tobacco smoking reached its peak in the notional West, engineers found technical solutions for supply and exhaust ventilation, which provided smoking and non-smoking areas within the same bar or restaurant.
It should be admitted that we, hygienists, often used purely arithmetic methods to derive the required indoor air exchange rates in terms of CO2 accumulation, without thinking about energy efficiency and technical capacity in terms of permissible supply and exhaust air flow rates and temperatures. In the real conditions of the energy crisis, it is almost impossible without air recirculation, especially in the cold season. However, hygienists still legally prohibit air recirculation, especially in hospitals. Nowadays, technical solutions have been found that allow recirculation systems to be used even in healthcare facilities by filtering the air through, for example, HEPA filters and using the bactericidal properties of ultraviolet radiation. How often have we thought about how people on space stations and submarines are supplied with air for many months? That is, there are technical solutions, and when society grows to understand the need to combat at the state level not only the economic consequences but also the impact of SARS epidemics on public health, appropriate developments will appear to organize air exchange in residential and public buildings.
The spread of aerosols containing viruses depends on the air exchange in the room and the ventilation system of the entire building. It should be noted that the natural ventilation system in multi-story residential buildings is capable of spreading virus-contaminated air between floors. Specific requirements have been developed for ventilation efficiency, both in terms of CO2 concentration and the volume of air to be supplied per person. Most people cannot control this, but it is worth remembering that not only through ventilation but also corner ventilation of the apartment, especially in the cold season, is quite effective. It takes 3-5 minutes to ventilate the room. Let us remind you once again: for natural ventilation to work in an apartment, there must be access to fresh air from the outside (an open window or window sash) and free paths (open doors) for air to move to the exhaust holes in the bathroom, toilet, and kitchen. Mechanical ventilation is more effective as a means of combating the spread of infection in the apartment and the building as a whole.
In analyzing the above article, we tried to emphasize the latest fundamental scientific understanding of the mechanisms of formation of a fine aerosol in the human respiratory system, which may contain viruses, and the most likely ways of transmitting this infectious agent from a person with SARS to a healthy person.
Although it is believed that COVID-19 has already moved to the list of seasonal viral respiratory infections, I would advise everyone to use all possible means and knowledge to avoid this disease in different climatic seasons.
Doctor of Medical Sciences, Professor
Akimenko V.Y.
State Institution «Marzieiev Institute for Public Health of the National Academy of Medical Sciences of Ukraine»
(date of publication on the website 17.01.2025)